Our research adopts a life-course model applying methods of health economics evaluation to trials and other study designs in the evaluation of public health and psychosocial interventions at both programme and system level. Our research has applications within the NHS, third sector organisations, and government. Much of our research is funded by NIHR, HTA, charities, and Welsh Government.
With a research and policy lens, we apply health economics to public health and prevention, well-being and well-becoming. For example, we have published three reports commissioned by Public Health Wales: Transforming Young Lives across Wales; Wellness in Work; and Living Well for Longer. The full reports are available below:
Our expertise and the methods we use are displayed in this infographic:

Image description: This is a spider graph detailing the methods we use. The categories form a concentric ring in blue, and they are: Social Value, Reviewing, Economic Evaluation, Participant-Centred and Prioritisation. The methods are displayed in red circles attached to each category. For Social Value they are social return on investment and return on investment. The methods for Reviewing are realist synthesis, systematic reviews and rapid reviews. Our economic evaluation methods are cost-effectiveness analysis, cost-consequence analysis, cost benefit analysis, Markov Modelling and cost-utility analysis. Participant-centred methods are realist evaluation and discrete choice experiments. Prioritisation methods are multi-criterial decision analysis and programme budgeting and marginal analysis.
International evidence points towards the greatest return on investment coming from investment in the first three years of life. Our research shows that positive preventative actions during child development are the most important ways to intervene and yield the greatest return on investment to society.
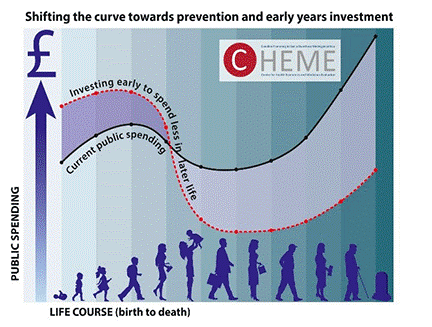
Image description: This image shows two graphs of public spending on health. The first curved line represents current public spending which increases over life course. The second line shows an alternative model investing early to spend less in later life.
Our Well-being and Well-becoming Wheel infographic shows how factors impact well-being through the life-course.

Image description: This infographic reflects an underlying concept of “the wheel of life”. The first concentric ring is red and reflects personal factors that determine or have an impact through the life-course on well-being and well-becoming. These are: employment and career; purpose and contribution; mental health; physical health; relationship and social connection; food , water and energy security; education and growth; personal identity; financial stability, and home and work environment. The second concentric ring is green and reflects local factors that determine or have an impact on well-being and well-becoming through the life-course. These are: national and local government policy; access to housing and transport; access to education and employment; neighbourhood, built and natural environment; access to green and blue spaces; access to health and social care, health literacy and justice. The third concentric ring is blue and reflects national and global factors that determine or have an impact on well-being and well-becoming through the life-course. These are: environmental and climate change, social and cultural norms; technology; globalisation; macroeconomic conditions; geo-political conditions, and war, terrorism, famine, pandemics and natural disasters.
The impact of our research activities is far-ranging, as shown in the infographic below.

Image description: This is a spider graph demonstrating our impact. It is formed of eight circles coloured in orange and blue. They are research outputs and publications, influencing policy, teaching and skills, informative resources, identifying preventative health measures, demonstrating return on investment, addressing societal issues, and collaboration and building networks.
Our research attracts funding from a variety of sources, as shown in our infographic:
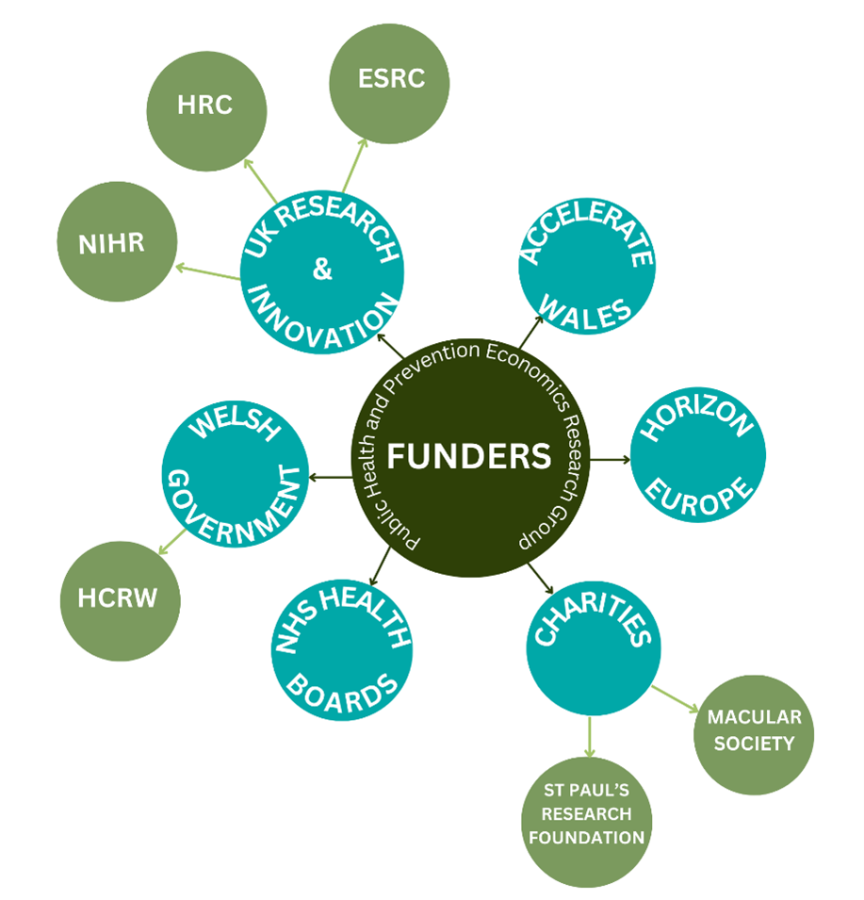
Image description: This is a spider graph showing our funding sources. There are six funding sources shown as blue circles. They are the UKRI which includes smaller connected green circles for NIHR, HRC and ESRC, Welsh Government which includes a smaller connected circle for HCRW, charities which include green circles for the Macular Society and St Paul’s Research Foundation, NHS health boards, Horizon Europe and Accelerate Wales.
AdaptQoL: Adaptation and Quality of Life
The aim of the AdaptQoL project is to develop a new patient-reported outcome measure (PROM) for assistive technology users. PROMs are questionnaire tools commonly used to measure individual health outcomes, like quality of life and symptom management. Sometimes PROMs are preference-based, which means that they reflect patient or societal preferences for different states of health. In this project we aim to develop a new preference-based PROM which will support health economists, clinicians, therapists and patients to accurately measure the quality of life benefits of different assistive technologies, both for the purpose of informing patient care and informing decision-making.
The AdaptQoL project will run until April 2027 and is funded by the Welsh Government through Health and Care Research Wales.
Horizon Europe Invest4Health
The Centre for Health Economics and Medicines Evaluation (CHEME) are key partners in the EU Invest4Health project. This Horizon Europe collaboration across eight countries has been funded as one of the four large research programmes on the HORIZON-HLTH-2022-CARE-08-04 — Better financing models for health systems call. CHEME’s key contribution to this project include exploring what is meant by Smart Capacitating Investment (SCI), across the public, private and voluntary sectors at a macro, meso and micro level, and testing and evaluating proposed SCI models that aim to provide sustainable funding for preventive health measures in the post-COVID-19 healthcare landscape.
Advice on Prescription
Citizens Advice on Prescription (CAP) is a welfare and social prescribing intervention provided by Citizens Advice Liverpool Health Programme | Citizens Advice (citizensadviceliverpool.org.uk). The aim of CAP is to provide a single ‘gateway’ from health services in Liverpool into a holistic social and welfare support offer. A key element of the CAP service is that it is designed both to improve the lives of individuals, but also provide support for the health care system, with the aim to reduce the pressures from non-health issues on the health service.
The public health economics team, in conjunction with The University of Liverpool, are currently evaluating the effectiveness and cost-effectiveness of the CAP program. For the health economic analyses, we will be using health related quality of life (HRQOL) utility values as well as changes in health service usage (e.g., number of GP and hospital visits), and program costings to carry out a cost effectiveness analysis (CEA) and social return on investment (SROI) on the intervention.
Methodology of public health economics
Edwards, R. T., & McIntosh, E. (Eds.). (2019). Applied health economics for public health practice and research. Oxford University Press. This book is the fifth in the series of Handbooks in Health Economic Evaluation.

- In 2022 we hosted a free, online 2-day course to accompany our textbook. The course attracted over 150 delegates worldwide from around 60 organisations.
- Edwards, R. T., & Lawrence, C. L. (2021). ‘What You See is All There is’: the importance of heuristics in cost-benefit analysis (CBA) and social return on investment (SROI) in the evaluation of public health interventions. Applied Health Economics and Health Policy, 19(5), 653-664
Policy Support
We deliver health economics advice and support to health and social care organisations in accordance with Welsh Government priorities and needs. For example:
- Through our work with the Health and Care Research Wales Evidence Centre we collaborate closely with Public Health Wales and other stakeholders such as Welsh Government on rapid reviews of the available health and social care evidence. Recent reviews include wellness of the workforce and models of palliative care (in progress).
- Rhiannon led the Bangor Institute for Health and Medical Research (BIHMR) team as partner in the Wales COVID-19 Evidence Centre, which has led to a new £5 million grant led by Cardiff, as a reviewing centre for Welsh Government to support evidence-based policy in health and social care post-pandemic. These include rapid reviews on the effectiveness and cost-effectiveness of interventions in reducing harms for children and young people who have been exposed to domestic violence/abuse, and interventions and best practices to support people with long-COVID to return to normal activities.
- Rhiannon acted as an expert to the Office of Welsh Affairs for UK Government on potential scarring of the Wales economy post-pandemic.
Health economics of well-being and well-becoming
Upcoming: Oxford University Press (OUP) book – Health economics of well-being and well-becoming across the life-course
- Invest4Health, led by the University of Gothenburg, funded by Horizon Europe.
- Ways-to-Wellbeing, funded by The Health Foundation and NIHR.
- New therapeutic coaching approach for improving emotional wellbeing (EMD coaching), in collaboration with Cardiff University, funded by the Accelerate Programme (via the CHEME Social Value Hub).
- The Outdoor Partnership: '‘Opening Doors to the Outdoors’ (ODO) Programme, in collaboration with Cardiff University, funded by the Accelerate Programme.
- The Fathom Trust Making Well Green Social Prescribing Programme, funded by Cardiff University.
- Well-being and well-becoming through the life-course in public health economics research and policy: A new infographic.
Research projects and collaborations through the life-course
Early years and childhood
- Speak Out Stay Safe (SOSS) programme, in collaboration with the University of Central Lancashire, funded by NSPCC. View the summary report. (Please note: a fully accessible version of this document will be available soon.)
Adolescents and young people
- KiVa trial: The effects and costs of an anti-bullying programme in UK primary schools: a multicentre cluster randomised controlled trial, led by Bangor University, funded by NIHR.
- Choosing Active Role Models to Inspire Girls (CHARMING), in collaboration with Cardiff university, funded by Health and Care Research Wales, Welsh Government.
- Exploring the barriers and enablers to services for young people who are care-leavers: a qualitative study, funded by Health and Care Research Wales.
Working age
- Evaluating the health impact and cost-effectiveness of Ways-to-Wellbeing, a whole system approach to mitigate poverty over the life course, in collaboration with the University of Liverpool, funded by NIHR.
- Shared Roadmap for System Change, in collaboration with the University of Central Lancashire, funded by Women’s Aid and Safer Lives.
- MAP ALLIANCE Optimising care for perinatal anxiety: Evaluation of health service utilisation, outcomes and costs, in collaboration with City, University of London, funded by NIHR.
Older age – living well for longer
- Trio Shared Lives (short breaks for people with dementia), led by Bangor University, funded by Health and Care Research Wales, Welsh Government.
- Promoting Activity, Independence and Stability in Early Dementia (PrAISED) research programme, in collaboration with the University of Nottingham, funded by NIHR.
- A randomised controlled trial and feasibility study of the effects of an e-health intervention ‘iSupport’ for reducing distress of dementia carers, especially in the ongoing pandemic of COVID-19, led by Bangor University, funded by NIHR.
- The impact of peer support networks for those living with rare dementias, in collaboration with University College London, funded by ESRC and NIHR.
Where and how we die well
- Funding and access to hospice care in Wales: A North Wales case study.
- What available evidence is there on the costs and cost-effectiveness of different service models of palliative care, with a focus on end-of-life care? [working title]. A rapid review for the Wales Evidence Centre.
Evaluation of medical devices and technologies
- Clinical Development of an Ultrasensitive OCT Device to Improve the Management of Eye Disease, in collaboration with the University of Liverpool, funded by HTA.
Economic evaluation of sight loss and sight preserving surgery
- Access to counselling during sight loss survey, led by Bangor University, funded by North Wales Society for the Blind.
- Adjunctive Steroid Combination in Ocular Trauma (ASCOT), in collaboration with Moorfield’s Eye Hospital and King’s College London, funded by NIHR.
We offer a Master by Research in Public Health and Prevention Economics.
Medical students at the North Wales Medical School, Bangor University
- Rhiannon offers a student selected component (SSC) for 2nd to 4th year students - ‘Public health and prevention economics research across the life-course’ experience project. Students will have an opportunity to join the Public Health and Prevention Economics Research network at CHEME.
Bespoke lectures on public health economics and related topics
- Rhiannon provides lectures for the following:
- Module NHS-4003 Introduction to the Principles of Health Economics as part of the MSc in Public Health and Health Promotion course at Bangor University.
- Bangor University Health Services Research Summer School.
- Master of Public Health course at the University of Liverpool.
Professor Rhiannon Tudor Edwards – Professor of Health Economics, Co-Director of CHEME, and Co-Director of Health and Care Economics Cymru (HCEC)
Ann Lawton – Operational Manager and Administrator
Dr Ned Hartfiel – Research Fellow in Health Economics and Co-Lead for the CHEME Social Value Hub
Dr Ceryl Davies – Senior Research Fellow
Dr Victory Ezeofor – Mathematical/Statistical Modeller in Health Economics
Dr Bethany Anthony – Research Officer in Health Economics
Dr Sofie Roberts – Research Officer in Health Economics (on maternity leave)
Dr Huw Lloyd-Williams – Research Officer in Health Economics
Dr Hannah Jelley – Research Officer
Jacob Davies – Research Project Support Officer
Pim Doungsong – Research Project Support Officer
Kalpa Pisavadia – Research Project Support Officer
Greg Flynn – Research Project Support Officer
Anusha Singh – Research Project Support Officer
- Dr Jo Davies – Deputy Head of Health Economics, Finance Directorate, Health and Social Services Group, Welsh Government
- Dr Gethin Griffiths – Director of Outcomes Research, GSK
- Dr Natalia Ivashikina – Senior Lecturer in Global Health Economics, Brighton and Sussex Medical School
- Dr Huw Lloyd-Williams – Research Officer, CHEME, Bangor University
- Abraham Makanjuola – Research Assistant, University of South Wales
- Alan Ó Céilleachair – Researcher, University College Cork, Ireland
- Dr Laura Ternent – Senior Lecturer, Newcastle University
- Dr Laura Timmis – Research Officer, CHEME, Bangor University
- Alex Torbuck – PhD candidate, University of Rochester, New York
- Dr Sayed Ramin Ziwary – The World Bank Young Professional Program
- Sharon Hadley, Oxford Mindfulness Centre
- Professor Stephen Robson, leader in health and health policy in Australia
- Dr Vladyslav Kulikov, MD
- Dmytro Babelyuk, MD, lecturer at Arden University, London
- Eira Winrow, Lecturer in Health Sciences at Bangor University
- Jacob Davies, Research Project Support Officer at CHEME
- Kalpa Pisavadia, Research Project Support Officer at CHEME
- Pim Doungsong, Research Project Support Officer at CHEME
PHERG supports Bangor University’s mission to create an active workplace to support the health and well-being of colleagues. Our short film below shows how PHERG is achieving excellence in research and teaching in the area of health economics of prevention and public health through an active workplace.
Our short film can be found on the CHEME YouTube channel http://www.youtube.com/@CHEME-bangoruni




